Control Pause – Measure Your Carbon Dioxide Threshold
The Control Pause (CP) is an assessment of your breathing pattern. If your CP is less than 25 seconds, it indicates that your breathing has room for improvement. If your CP is above 25 seconds, there is an 89% chance that your breathing is functional.
The measurement is based on how long you can hold your breath after exhaling. Using the Control Pause to measure your progress with the Buteyko Breathing Method, means you can reliably improve your carbon dioxide threshold, leading to better all-round health. As your Control Pause increases, your breathing pattern is improving.
Every time your Control Pause increases by 5 seconds, your breathing pattern improves and you will feel better. People with a low Control Pause of between 5 and 15 seconds, typically breathe with a faster respiratory rate, more upper chest, have irregular breathing and often feel like they cannot take a deep breath.
The Control Pause measurement is influenced by your sensitivity to the build-up of carbon dioxide in the blood. As you practice the Buteyko Method, your sensitivity to carbon dioxide reduces. This in turn enables you to hold your breath for longer.
The Buteyko Control Pause will provide you with feedback on your symptoms, and most importantly, your progress. E.g. people with asthma, rhinitis, high stress, anxiety, etc. will continue to experience symptoms as long as their Control Pause is less than 20 seconds.
How to Measure Your Control Pause

- Take a small, silent breath in and out through your nose.
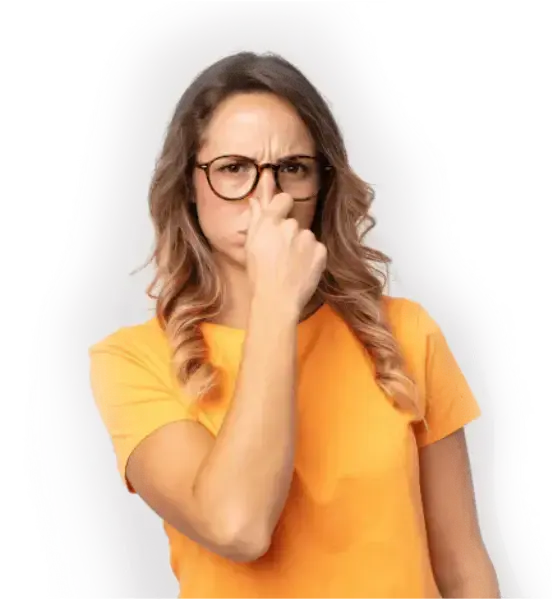
- After the exhaling, pinch your nose with your fingers to stop air from entering.
- Use a timer to count the seconds until you feel the first real need to inhale.
- Release your nose and breathe normally through it. Control Pause Measurement Instruction
A few things to keep in mind before you start…

- To The Buteyko Breathing Control Pause is a measurement of your breath-hold time only. It is not an exercise to correct your breathing.
- Once you experience the first involuntary movements in your breathing muscles or throat, or the first physiological urge to breathe, do not continue to hold your breath any longer.
- If your first inhalation after the breath hold is big, audible, or uncontrolled, it is likely that you’ve held your breath for too long.
- For the most accurate results, measure your Control Pause first thing in the morning.
What Your Control Pause Measurement Means
A low Control Pause means a low breath-hold time and poorer breathing patterns. When breathing patterns are poor, or if the individual is overbreathing, this can impact their health. E.g. They become more prone to asthma symptoms such as coughing, wheezing and breathlessness. They also are more prone to snoring and sleep apnea as well as anxiety and panic disorder. This depends on genetic predisposition.
If you are affected by these conditions and your Buteyko Breathing Control Pause remains low, you will continue to experience these symptoms. Over the years, we have found that when people improve their Control Pause, their asthma symptoms, sleep disorder breathing, anxiety and panic disorder reduce significantly.
Each time your Control Pause increases by 5 seconds, you will feel better. Aim for a 3 or 4 second increase each week for the first few weeks, but don’t feel disappointed if it doesn’t continue to change. Sometimes the Control Pause will plateau. Keep practicing and it will change for the better.
Do You Have a Good Control Pause?
- Poor: Less than 15 seconds.
- Room for improvement: Between 15 and 25 seconds.
- Good: Above 25 seconds.
- Great: 40+ seconds.
Relationship Between Breathing Volume and Control Pause




Three Steps to Improve your Control Pause:
- Stop “Big Breathing” using the following tips:
- Close your mouth, breathe in and out through the nose.
- Apply calm and gentle, reduced volume breathing.
- Aim for silent breathing during rest and sleep.
- Practice reduced breathing exercises.
- Breathe through the nose while taking physical exercise. To increase the CP from 20 to 40 seconds, it is necessary to add physical exercise to the breathing exercises.
Your Control Pause: What the Science Says About the Control Pause as a Measure of CO2 Tolerance
As far back as 1975, researchers Stanley et al. noted that breath holding was a simple test to determine respiratory chemo sensitivity and concluded that, “the breath hold time/partial pressure of carbon dioxide relationship provides a useful index of respiratory chemo sensitivity which is not influenced by airways obstruction.”
valuation of breath holding in hypercapnia as a simple clinical test of respiratory chemo sensitivity. Stanley,N.N.,Cunningham,E.L., Altose,M.D.,Kelsen,S.G.,Levinson,R.S., and Cherniack,N.S.(1975).Thorax,30,337-343.
In another paper, Nishino acknowledged breath holding as one of the most powerful methods to induce the sensation of breathlessness, and that the breath hold test, “gives us much information on the onset and endurance of dyspnea (breathlessness).”
The paper noted that two different breath hold tests provided useful feedback on breathlessness. The first breath hold test simply measures the length of time until the first urges to breathe begin. This easy breath hold provides information of how soon the first sensations of breathlessness take place, and was noted to be a very useful tool for the evaluation of dyspnea.
The second measurement is the total length of the breath hold time. This provides feedback on the upper limit toleration of breathlessness and is influenced by behavioral characteristics such as willpower and determination. As the first test is not influenced by training effect or behavioral characteristics, it can be deduced that it is a more objective measurement.
Respir Physiol Neurobiol. 2009 May 30;167(1):20-5. Epub 2008 Nov 25. Pathophysiology of dyspnea evaluated by breath-holding test: studies of furosemide treatment. Nishino T.
Eighteen patients with varying stages of cystic fibrosis were studied to determine the value of the breath hold time as an index of exercise tolerance. The breath hold times of all patients were measured. Oxygen uptake (Vo2) and carbon dioxide elimination was measured breath by breath as the patients exercised. The researchers found a significant correlation between breath hold time and VO2 (oxygen uptake), concluding “that the voluntary breath-hold time might be a useful index for prediction of the exercise tolerance of CF patients.”
Eur J Appl Physiol. 2005 Oct;95(2-3):172-8. Epub 2005 Jul 9 Relationship between breath-hold time and physical performance in patients with cystic fibrosis. Barnai M, Laki I, Gyurkovits K, Angyan L, Horvath G.
Results from a study of 13 patients with acute asthma, concluded that the magnitude of breathlessness, breathing frequency and breath hold time correlated with severity of airflow obstruction and secondly breath hold time varies inversely with dyspnea magnitude when it is present at rest.
Rev Invest Clin. 1989 Jul-Sep;41(3):209-13. Rating of breathlessness at rest during acute asthma: correlation with spirometry and usefulness of breath-holding time. Perez-Padilla R, Cervantes D, Chapela R, Selman M.
In other words, the lower the breath hold time, the greater the volume of breathing of asthmatics at rest.
Easy Breath Holds vs. Maximum Breath Holds
When determining the usefulness of breath hold tests, it is necessary to take into consideration subjective influences. In other words, individuals with strong willpower can hold their breath for longer than those without. Therefore, breath hold time provides more accurate feedback if subjective influences can be removed.
Holding of the breath until the first involuntary movements of the breathing muscles provides more objective feedback on relative over-breathing.
In a study of 13 normal subjects who performed repeated breath holds, results showed that holding of the breath until the first respiratory sensations does not create a breath hold stress, and so is less influenced by the training effect. Authors also noted that holding the breath until the first breathing sensation is “inversely related to the slope of the hypercapnic ventilatory response curve,” and so provides a very useful diagnostic tool of breathlessness.”
Clin Sci (Lond). 1996 Dec;91(6):755-61. Changes in the period of no respiratory sensation and total breath-holding time in successive breath-holding trials. Nishino T, Sugimori K, Ishikawa T.
